- Necrotizing fasciitis
- A dangerous infection of soft-tissue that starts in the subcutaneous tissue (just below the skin) and spreads along the flat layers of fibrous tissue that separate different layers of tissue (fascial planes). It most commonly occurs in the arms, legs and abdominal wall. The death rate is up to 40%. Necrotizing fasciitis can be caused by only one type of bacteria (monomicrobial) or by a combination of bacteria such as E. coli and Bacteroides fragilis or clostridium (polymicrobial). Monomicrobial infections account for 10% and polymicrobial for 90% of cases of necrotizing fasciitis. Symptoms include redness (erythema), swelling (edema) and tenderness. The degree of pain typically is greater than the severity of these findings and the person appears terribly ill. The original skin wound is often evident. Skin changes may include bullous lesions (blisters) and local skin anesthesia (due to blocking of little vessels in the skin). A crinkly or crackling feeling called crepitus indicates gas in the tissues but occurs in only about half of cases. Emergency diagnosis and treatment are essential. Broad-spectrum antibiotic treatment and prompt surgical removal of dead and infected tissue decreases the death rate.
* * *
necrotizing fasciitis n a severe soft tissue infection typically by Group A streptococci or by a mixture of aerobic and anaerobic bacteria that is marked by edema and necrosis of subcutaneous tissues with involvement of the fascia and widespread undermining of adjacent tissue, by painful red swollen skin over affected areas, and by polymorphonuclear leukocytosis and that usu. occurs as a complication of surgery, injury, or infection by extension from the initially affected site* * *
bacterial infection of the layer of fascia beneath the skin by Streptococcus Type A. There is tissue necrosis and toxin production causing shock and organ failure. Symptoms appear rapidly after initial infection; they include a rash with blistering and discoloration of the skin, pain and inflammation of lymph nodes, fever, drowsiness, diarrhoea, and vomiting. The elderly and those who have recently undergone surgery are particularly vulnerable to the infection, which requires prompt treatment with antibiotics (e.g. clindamycin) and excision of the involved tissue.* * *
a fulminating subcutaneous soft tissue infection beginning with extensive cellulitis that rapidly spreads to involve the superficial and often the deep fascia, producing thrombosis of subcutaneous vessels and gangrene of the underlying tissues. A cutaneous lesion often serves as a portal of entry for the infection. Although the infection is most closely linked to group A streptococci, it can be caused by other bacteria, either alone or in combination, and is categorized based on the infectious agents isolated. Polymicrobial infections with aerobic and anaerobic organisms are type 1, infection by group A streptococci is type 2, and gas gangrene is sometimes considered to be type 3. Called also gangrenous or necrotizing cellulitis and gangrenous or necrotizing erysipelas.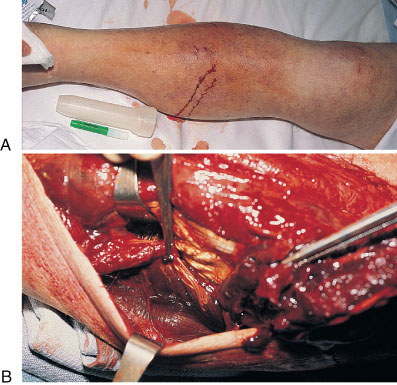
 Necrotizing fasciitis caused by group A streptococci in a 60-year-old man with diabetes mellitus type 2. (A), The calf is swollen but the skin looks relatively normal except for two small purple bullae. (B), Surgical view shows extensive necrotizing fasciitis with myonecrosis beneath the fascia.
Necrotizing fasciitis caused by group A streptococci in a 60-year-old man with diabetes mellitus type 2. (A), The calf is swollen but the skin looks relatively normal except for two small purple bullae. (B), Surgical view shows extensive necrotizing fasciitis with myonecrosis beneath the fascia.
Medical dictionary. 2011.
